
EPC Statement on Palliative Care and Voluntary Assisted Dying
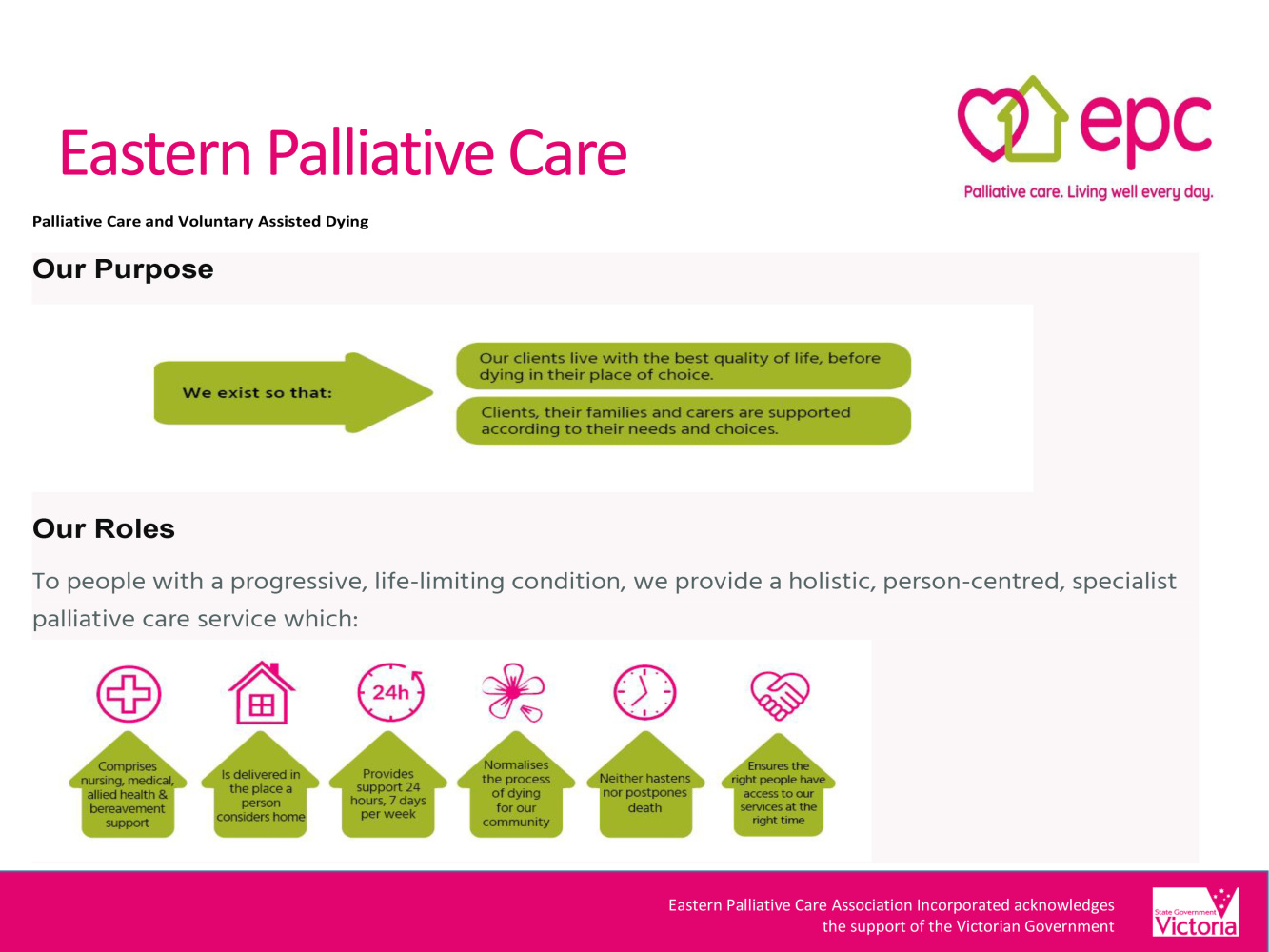
Palliative Care:
- Affirms life and regards dying as a normal process
- Neither hastens nor postpones death
- Provides relief from pain and other distressing symptoms
- Integrates the physical, psychological, social, emotional and spiritual aspects of care
- Offers a support system to help people live as actively as possible until death
- Offers a support system to help the family cope during the person’s illness & their own bereavement
- Palliative care is provided to people of all ages who are dying.
Our response to Voluntary Assisted Dying (VAD)
At EPC we are deeply committed to provide you, your carers and family with high quality, person-centred care, support and accompaniment so that you live well every day.
In June 2019, VAD came into effect in Victoria. Victorians who are at the end of life, and who meet strict eligibility criteria, can request access to the VAD Program. Following a series of assessments, a person in the late stages of advanced disease can take medication, prescribed by a doctor, that will bring about their death at a time they choose.
EPC’s commitment to your care does not include the deliberate ending of life, because it conflicts with our model of palliative care. Palliative Care neither prolongs nor hastens the dying process. EPC’s role is not to influence when death will occur. We oppose, and do not participate in, Victoria’s VAD Program. Therefore, our staff are not involved in either the VAD assessment processes, nor the preparation or taking of VAD medication. However, we will not discriminate in the care we provide to clients who are considering VAD or going through that process.
In no way does our position on VAD exclude anyone from EPC’s program and the normal care and services we provide. We invite open discussion with you and your family about your values, goals and the nature of suffering and illness. We will provide high quality symptom management and palliative care that respects your preferences. EPC’s role as a specialist community palliative care service will always be to relieve your suffering and discomfort and provide person-centred care in the natural process of dying.




 Make a Referral
Make a Referral